Table of contents
Cysts are benign growths composed of fluid or solid materials that may contain liquid, “cheese,” or chunky matter and can form anywhere on the body. They may appear anywhere.
Noncancerous cysts such as the benign pseudocyst and serous cystadenoma should not cause symptoms or grow larger, although cancerous or precancerous cysts should be drained and surgically removed as soon as possible.
Treatment of Pancreatic Cyst
Pancreatic cysts span benign pseudocysts to malignant types. Treatment varies by cyst type, size, and symptoms. Options include:
- Monitoring: Small, symptom-free cysts might be observed with regular imaging tests.
- Drainage: Larger or symptomatic cysts may require drainage via endoscopy, catheter, or surgery.
- Surgery: Surgery can remove certain cysts, notably cancerous or pre-cancerous ones, with techniques like open, laparoscopic, or robot-assisted surgery.
- Total Pancreatectomy: Extensive cyst impact might lead to total pancreas removal, necessitating lifelong insulin and enzyme supplements.
Discuss with your doctor to decide the best approach for your specific case.

Medical Treatment
Pancreatic cysts can typically be identified through imaging studies like MRI or CT scans or during surgery for another condition. They may also be detected via endoscopic ultrasound – an endoscope-guided ultrasound procedure involving inserting a thin tube with a camera into your mouth and down through your digestive tract to view the pancreas directly.
Most benign cysts don’t require treatment unless they cause symptoms; those which do may need to be drained off.
Mucin-producing cysts that are precancerous – including intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystadenomas – should be surgically removed due to their potential to progress into cancerous tumors.
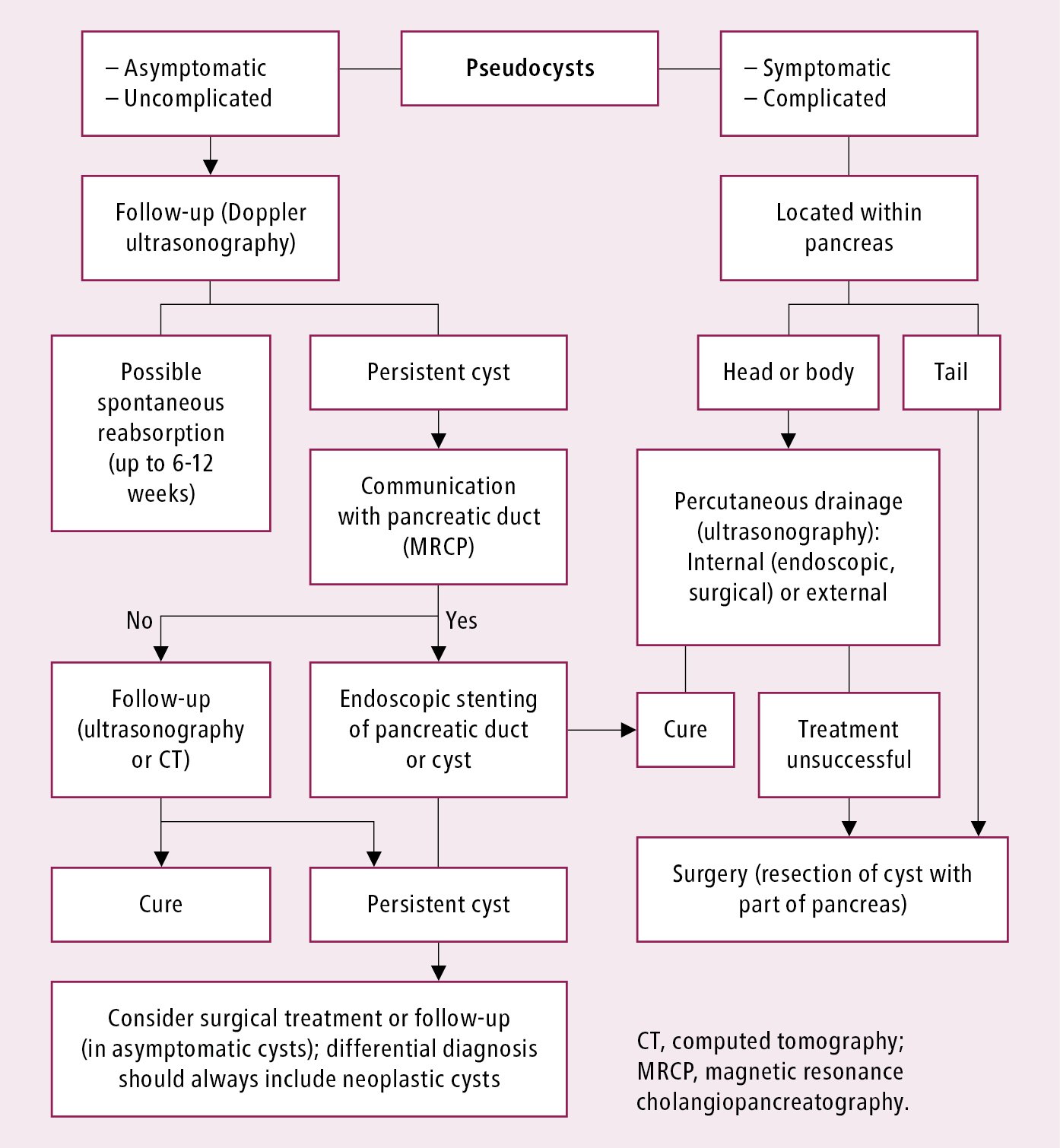
Pseudocysts, composed largely of fluid, are a common complication of pancreatitis. They form when inflamed pancreatic cells release enzymes into the surrounding tissue which damage its integrity.
Many pseudocysts will heal without drainage while larger and symptomatic ones need to be drained either percutaneously or using endoscopic retrograde cholecystography – which involves inserting a tube directly into your stomach – either of these methods should be employed.
Endoscopic Ultrasound
Most benign pseudocysts will clear on their own without intervention; however, when symptoms arise or high risk features are detected on imaging, doctors can perform endoscopic ultrasound-guided fluid sample (endosonography) or percutaneous drainage as a means to manage these cysts.
For this test, physicians use an endoscope, which is a lighted tube inserted through your mouth into your digestive tract and down past your stomach. It allows them to observe the lining of intestines and pancreas as well as any abnormal cells within your body.
They may even use this instrument to pass needle into cyst and collect sample of fluid for examination under microscope.
These samples help your doctor diagnose the type and condition of cyst, including whether it may be precancerous or cancerous.
Based on its results, your physician may suggest additional imaging tests, endoscopies/biopsies/surgery removal as necessary; in particular if it involves mucin-producing lesions like an intraductal papillary mucinous neoplasm which has been associated with malignancy; it would likely be surgically removed by default.
Surgical Drainage
Drainage is often the first step in treating pancreatic cysts caused by chronic pancreatitis (pseudocysts), particularly small ones without cancer risks.
An endoscopic drainage procedure allows doctors to take an examination of fluid inside of your cyst as well as obtain needle biopsy specimens using thin tubes with cameras attached through your mouth and into your stomach – this allows them to examine any fluid accumulation within them before performing endoscopic drainage or endoscopy.
If your pseudocysts are larger or symptomatic, our gastroenterologists may recommend surgery to remove them. Minimally invasive procedures like laparoscopic pancreatoduodenectomy or robotic-assisted surgery are commonly used.
For certain patients with serous cystadenomas or solid pseudo papillary neoplasms – which may grow large enough to cause pain or an abdominal mass – we may advise surgery in order to completely eliminate them. Our doctors are experienced at performing this procedure using advanced endoscopic techniques.

Surgical Excision
Many types of pancreatic cysts, including fluid collections called pseudocysts that form due to pancreatitis and serous cystadenomas that develop as benign lesions, are noncancerous and will go away on their own; others, like intraductal papillary mucinous neoplasms (IPMNs) may progress into cancerous masses that require medical intervention in order to be removed safely.
Your doctor will use imaging scans such as MRIs and CT scans to gain more information about your cysts. They may also perform endoscopic ultrasound (EUS), which involves inserting a lighted tube with a camera through your mouth into your stomach and digestive tract in order to get an up close and personal view of your pancreas.
Your doctor will likely monitor any type of cyst, cancerous or precancerous, that changes in size over time with imaging tests, endoscopies and taking fluid samples from it to observe for changes.
They could do this through imaging techniques such as CT or PET scans as well as taking fluid samples directly from it in order to check on cells changing within it.
What Are the Symptoms of Pancreatic Cysts
Pancreatic cysts often remain symptomless, concealing their presence. Yet, once they reveal themselves, symptoms manifest diversely, contingent on cyst size, location, and type. Common indicators associated with pancreatic cysts include:
- Abdominal pain: Pancreatic cysts frequently yield persistent abdominal pain. This discomfort localizes in the upper abdomen, occasionally radiating towards the back.
- Nausea and vomiting: Certain individuals afflicted with pancreatic cysts encounter bouts of nausea and vomiting.
- Abdominal bloating: Pancreatic cysts are capable of inducing abdominal bloating, evoking discomfort.
- Weight loss: Unexplained weight loss occasionally materializes in cases involving pancreatic cysts.
- Sensation of an abdominal mass: A subset of individuals may detect a mass or lump situated in their upper abdomen.
- Jaundice: In isolated instances, pancreatic cysts can incite jaundice, a manifestation characterized by skin and eye yellowing.
Significantly, these symptoms possess potential associations with other medical conditions. Consequently, seeking a healthcare professional’s expertise is crucial for obtaining an accurate diagnosis.
Should any of these symptoms emerge or concerns regarding pancreatic cysts arise, it is highly advisable to seek medical attention, facilitating thorough evaluation and informed guidance.
What Are the Different Types of Pancreatic Cysts

Pancreatic cysts come in multiple types, split into two groups: nonneoplastic or neoplastic. Here’s the breakdown:
Nonneoplastic cysts:
- Pseudocysts: Most common, caused by pancreatitis, filled with fluid and enzymes.
- Serous cystadenomas: Benign, hold clear, watery fluid.
- Lymphoepithelial cysts: Rare, lined with lymphoid tissue.
- Retention cysts: Form from blocked pancreatic ducts, filling with fluid.
Neoplastic cysts:
- Intraductal papillary mucinous neoplasms (IPMNs): Common, mucus-filled.
- Mucinous cystic neoplasms (MCNs): Filled with thick fluid, higher cancer risk.
- Solid pseudopapillary neoplasms: Rare, often benign but can turn cancerous.
- Cystic pancreatic neuroendocrine tumors: Uncommon, fluid-filled, linked to neuroendocrine tumors.
Remember, some cysts may show traits of more than one type. For precise identification, a biopsy or diagnostic test may be essential.

What Are the Risk Factors for Developing Pancreatic Cysts
Developing pancreatic cysts can involve varied risk factors. Most cysts’ exact causes remain unknown. However, specific factors heighten the chance. Here’s the breakdown:
- Pancreatitis: Inflamed pancreas elevates risk. Triggers include alcohol, gallstones, and injuries.
- Pancreatic cancer history: Past pancreatic cancer links to heightened cyst risk.
- Genetic disorders: Conditions like von Hippel-Lindau disease increase cyst risk.
- Abdominal trauma: After accidents, cyst formation becomes more likely.
- Gallstones and alcohol use: These heighten pancreatitis risk, in turn increasing cyst likelihood.
Remember, having these factors doesn’t guarantee cysts, while some develop cysts without clear factors. For concerns or symptoms, consult a healthcare expert for proper guidance.














