Table of contents
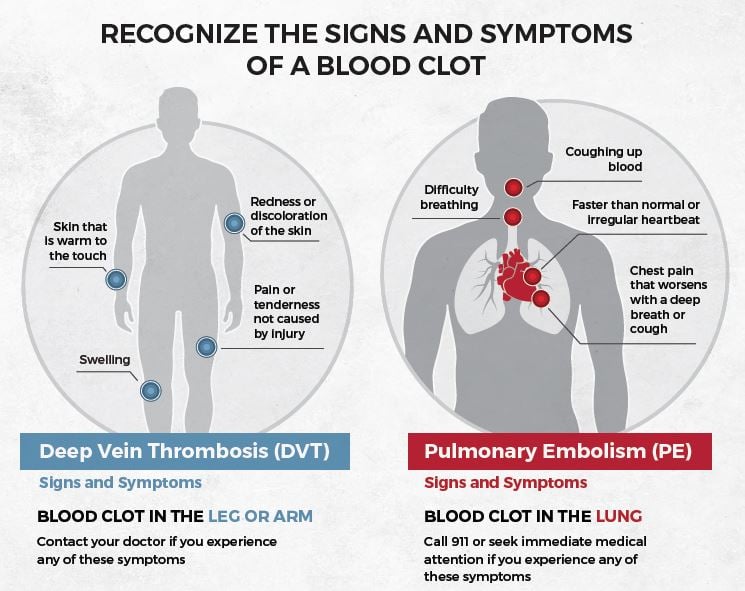
Blood clots can be life-threatening. Their symptoms depend on where and how big the clot forms; symptoms could include swelling of an arm or leg, pain that won’t go away, warm skin with red patches and changes to its color as well as skin changes that occur over time.
Clots that form in the deep veins of legs or arms can break off and travel to the lungs, leading to pulmonary embolism. If clots form in either your heart or brain they can also lead to serious complications – heart attacks or strokes being two potential outcomes of such events.

Symptoms of Blood Clots
Blood clots are serious and need quick treatment. Common symptoms:
- Swelling in a limb
- Leg pain or tenderness
- Skin discoloration
- Limb warmth
- Breathlessness, chest pain, coughing blood
- Sweating
- Nausea or vomiting
- Trouble breathing
- Chest pain
- Throbbing or cramping pain
- Warm skin around pain
- Itchy skin
- Ache to intense pain
- Cough
Note: Clots can occur with few/no symptoms; seek medical help if suspected.
Pain
Blood’s natural function is to clot after an injury has occurred, which allows it to stop bleeding quickly after cuts or scrapes have occurred. Unfortunately, it can also clot in veins causing deep vein thrombosis (DVT). If this blood clot reaches your lungs it could result in life-threatening problems called pulmonary embolisms (PE).
Blood clots in the legs often feel like severe cramps or charley horses, with an affected leg becoming swollen, tender and warm to touch – sometimes red or bluish in hue and often distinguishable from its counterpart.
Blood clots in the arms may be less frequent but still can be painful, swollen, reddened and warm to touch, feeling ropey over veins in your arms and causing them to ache or throb in that area.
Swelling
Blood clots that aren’t necessary can cut off oxygen to your heart and brain, leading to potentially life-threatening emergencies. When this clot travels to your lung it is known as pulmonary embolism (PE), with symptoms including chest pain, heavy chest feelin’ rapid heartbeat coughing up blood and clammy skin as telltale signs.
These symptoms should prompt a trip to your doctor immediately; he or she can use anticoagulant medication to restore proper blood flow and potentially save your life.
Your best defense against blood clots lies in walking around, moving your legs and feet while sitting, not smoking and taking blood thinners as directed by your doctor. Compression socks or garments may also help; talk to your physician about any risks or benefits they present.
Shortness of Breath
Blood clots that form in veins that deliver oxygen to your heart, lungs and brain can be life-threatening emergencies as they prevent your body from receiving enough oxygen, potentially resulting in stroke or heart attack.
Pulmonary embolisms (PEs), blood clots that originate deep inside your body (usually legs) and travel to your lungs, are extremely serious health threats that require immediate medical treatment. PEs could also be signs of heart disease or lung cancer.
These symptoms tend to be more serious if they only appear in one leg or arm, and should be treated by using medications designed to break them up or dissolve them, along with surgery that prevents further spread to your heart or lungs.
Nausea
Blood clots may not always pose an imminent threat, but if they break loose and travel to your lungs they could pose a fatal pulmonary embolism (PE).
These blood clots most frequently form in the deep veins of your arm or leg, although they can occur anywhere in your body. A clot can cause pain, nausea or vomiting, swelling and other symptoms in its location; if a clot breaks loose and travels to your lungs, you could experience chest pain as well as jaw, back, arm or neck discomfort as well as shortness of breath and feeling light-headed or faint.
Blood clots can be a serious health concern and should be addressed as soon as possible. Seek medical attention immediately if you exhibit any of the above symptoms; your physician may refer you to a hematologist, who specializes in treating blood disease.

Vomiting
When blood clots cause abdominal discomfort, vomiting may result. If bright red blood appears in your vomit, this should be considered an emergency situation and you should contact 911 immediately.
Blood clots may form in your arteries as well, which could potentially lead to stroke if one forms in an artery that leads directly to your brain. This risk increases significantly if you’re older, have high blood pressure, smoke regularly or have had prior strokes or blood clots as well as taking nonsteroidal anti-inflammatory drugs (NSAIDs) for extended periods.
If a blood clot forms under your skin in your leg or arm, you may notice that the affected area feels warmer than usual and experience pain as well as bruised or discolored patches in its vicinity.
What Are the Treatment Options for Blood Clots
Blood clot treatment is vital and varies by location and severity. Common options:
- Blood thinners (anticoagulants): Prevent clot growth, reduce risk of new clots. Enoxaparin, Fondaparinux, Coumadin/warfarin, Heparin.
- Compression stockings: Enhance leg blood flow, prevent swelling and new clots.
- Thrombolytic meds: Dissolve clots via IV or catheter; for severe cases due to bleeding risk.
- Catheter-directed: Catheter breaks up clot or delivers clot-dissolving drugs.
- Surgical thrombectomy: Surgically remove clot from vein/artery, especially in limbs.
Treatment tailored to individual cases; follow doctor’s advice, take meds as prescribed to prevent recurrence.
What Are the Side Effects of Blood Thinners Used to Treat Blood Clots
Blood thinners, or anticoagulants, treat blood clots. While effective against clots, they have side effects. Common blood thinner side effects:
- Excessive bleeding: Thinning delays clotting, causing bleeding. Signs: bloody urine or stool, severe bruising, lengthy nosebleeds, vomiting/coughing blood, sudden back pain.
- Bruising and rash: Most common effects.
- Diarrhea or constipation.
- Nausea and vomiting.
- Upset stomach and diarrhea.
- Hemorrhaging: Life-threatening; prompt medical attention needed. Blood thinners linked to excess bleeding from minor injuries.
Note benefits usually outweigh risks. Follow doctor’s orders, report side effects.
How Long Does It Take To Recover From a Blood Clot
Blood clot recovery time varies based on the case, clot severity, and treatment. Guidelines:
- Active treatment: About 3 months for VTE; varies per person.
- Hospital stay: Depends on clot severity and natural dissolution. Could be 0 to 1+ weeks.
- Medication: Normal activities resume days after treatment start; pain and swelling ease.
- Long-term symptoms: Most recover, but some have lasting issues like shortness of breath or scar tissue. DVT can lead to post-thrombotic syndrome, causing chronic swelling and pain.
- Prevention: Post-DVT, adopt healthy habits to prevent future clots.
Recovery varies; obey doctor’s orders, take meds to prevent recurrence. Talk to your doctor with concerns.














