Table of contents
As soon as a wound occurs, blood quickly changes from liquid into a gel-like mass known as a clot to stop excessive bleeding. Though necessary for health reasons, these clots may pose danger if they form where they shouldn’t or fail to dissolve naturally.
Anticoagulant medicines or “blood thinners,” to help prevent blood clots from forming, may be prescribed in order to lower your risk. This way, blood clots won’t form and form into harmful clots that obstruct bloodflow.
How Long Does It Take to Dissolve Blood Clots?
Blood clots may take weeks to months for dissolution, contingent upon size. Natural dissolution duration hinges on clot size and location. Various clot-dissolving treatments include:
- Anticoagulant medications: Also called blood thinners, they prevent new clots, allowing existing ones to dissolve over a few months.
- Thrombolytics: Administered via IV or directly into blood vessels, these drugs address serious cases like pulmonary embolism. Unlike blood thinners, they spur clot breakdown using plasmin activation, jumpstarting the body’s natural clearance process.
- Surgical thrombectomy: Typically for severe cases where prior treatments fall short, this procedure removes clots through catheter or surgery.
Importantly, self-attempted blood clot dissolution at home can pose risks and elevate the potential for life-threatening conditions. If you suspect a blood clot, immediate medical attention is crucial.

Size of the clot
Blood clots form naturally as part of our bodies’ natural response to injuries in order to stop bleeding, but sometimes they break loose and travel directly to the lungs in an extremely dangerous condition known as pulmonary embolism (PE) or deep vein thrombosis (DVT).
Medical interventions are sometimes necessary to dissolve a blood clot. Your doctor may recommend anticoagulant medication such as heparin or warfarin to thin your blood and help prevent new clots from forming, while simultaneously helping any non-emergency clots to dissipate on their own.
Other treatments include medications known as thrombolytics or “clot busters.” When taken within several hours of experiencing symptoms, these medicines rapidly dissolve clots.
Our interventional radiologists also utilize catheter-based procedures known as thrombectomy that deliver these drugs directly to clots – this lowers your risk for long-term complications like post-thrombotic syndrome (PTS), while treating PE or DVT that has not responded well to heparin or warfarin therapy.
Location of the clot
Blood clots that break loose from their original location can travel throughout the body and pose an extremely real danger, particularly if they reach critical organs such as the lungs and brain. Clots in arteries may lead to stroke; those in veins could trigger deep vein thrombosis (DVT) or pulmonary embolism (PE).
If your blood clot doesn’t respond to medication, medical interventions may be necessary. One such technique is known as Thrombolysis – this involves administering medication directly into clots via small cuts in your leg or thigh; they’ll insert a catheter and deliver medication directly into them.
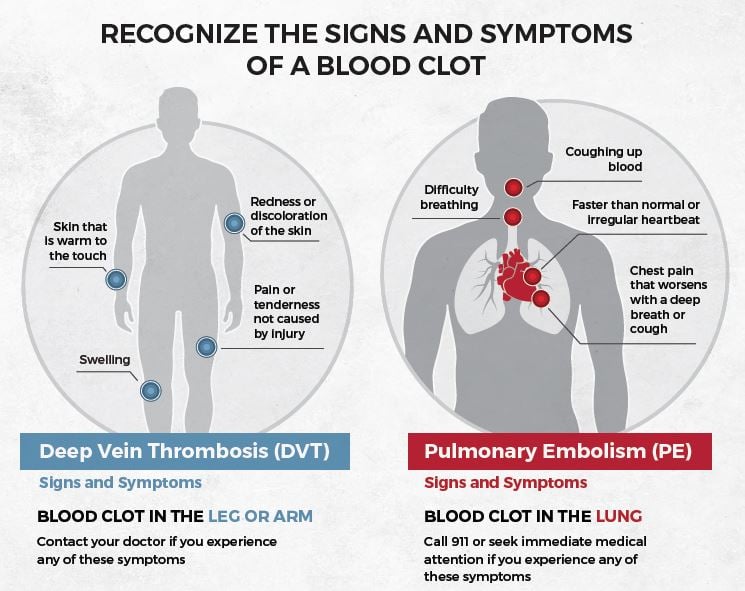
Blood clots in the arms or legs may result in swelling and redness, severe cramp-like pain, warm skin and fast or irregular heartbeat.
Other symptoms may include breathing difficulties, coughing up blood and feeling extremely heavy in your chest area – should any of these signs appear immediately seek medical advice! If this sounds familiar please call your physician immediately!
Underlying health conditions

Blood clots form to stop excessive bleeding when blood vessels are damaged, and usually dissolve once the injury heals. But sometimes clots form inside blood vessels causing problems like deep vein thrombosis (DVT) or pulmonary embolism (PE).
Doctors can prescribe medications known as clot-busters or thrombolytics to break up and dissolve blood clots, commonly referred to as “clot-busting”. A procedure called “thrombectomy” is also often performed to remove large blood vessel clots.
Conditions such as kidney disease can affect how quickly blood clots dissolve. Some medications, including hormone replacement therapy used by menopausal women, birth control pills and cancer treatment drugs, may increase your risk for blood clot formation.
Hematologists specialize in treating diseases of the blood, so they can help determine what’s causing blood clots and suggest treatments. Some options for DVTs and PE include medication to dissolve them or surgery to remove them, or anticoagulant medicines to prevent new ones forming.
Medications
Blood clots can be highly hazardous and lead to serious health issues like pulmonary embolism (PE) or heart failure, especially if left untreated quickly. They typically form in arteries connected to your heart and lungs and must be dealt with swiftly or they could become fatal.
As soon as a blood vessel becomes damaged, your body responds by turning flowing liquid into a gel-like mass called a clot to stop excessive bleeding. These clots typically break down and dissolve as the wound heals – but sometimes unexpected clots form and block blood flow throughout your body, potentially harming organs such as your brain or heart.
Medication may impact how quickly blood clots dissipate either naturally or with medical intervention, including anticoagulants and drugs known as thrombolytics that dissolve them quickly.
Recognizing Blood Clot Symptoms: What to Look For
Blood clot symptoms vary based on location and severity. Common indications include:
- Swelling: Often in one leg/arm, causing tenderness and enlarged appearance.
- Pain/tenderness: Presents as cramp or charley horse in affected area.
- Skin discoloration: Skin may turn reddish or bluish over clot.
- Warmth: Affected area feels warmer to the touch.
- Breathing difficulty: Pulmonary embolisms (lung clots) lead to breathing troubles; seek immediate help.
- Chest pain: Deep breaths or coughing worsening chest pain could suggest lung clot.
- Coughing blood: Lung clots might lead to coughing, even blood in severe cases.
Remember, these symptoms could arise from other issues too. Accurate diagnosis necessitates consulting a healthcare professional. If you suspect a blood clot, urgent medical attention is vital.
What Are the Risk Factors for Developing Blood Clots
Common risk factors for blood clots include hospitalization, major surgery (especially pelvis, abdomen, hip, or knee), severe trauma, vein injury, hip/knee replacement, cancer and treatments, estrogen birth control use, pregnancy/postpartum, estrogen hormone therapy, family history, overweight, immobility, prolonged sitting (legs crossed), smoking/vaping, age 55 or older, and long-term diseases.
Note: These factors don’t guarantee clots, but awareness aids prevention and seeking medical attention if necessary.

How Can Blood Clots Be Prevented
Preventing blood clots involves lifestyle changes and medical measures. Consider these tips:
Stay active: Regular exercise enhances blood flow; aim for 30-minute sessions most days.
Maintain a healthy weight: Managing weight via diet and exercise curbs clot risk.
Stay hydrated: Ample water thwarts clot formation by preventing blood thickening.
Quit smoking: Stopping smoking is vital, as it heightens clot risk.
Use compression stockings: These aid by preventing leg blood pooling, often doctor-recommended for at-risk individuals.
Take prescribed meds: Medications like blood thinners hinder clot formation and dissolution. Follow healthcare guidance.
Avoid prolonged sitting: Prolonged sitting ups clot risk, especially during flights or road trips. Move every hour to boost blood flow.
Note that some individuals may face higher clot risk due to medical issues or genetics. Consult your doctor for tailored precautions.














