Table of contents
Blood clots in your lungs can be an acute medical emergency. They can be extremely painful and lead to breathing issues as well as heart failure.
Your doctor will likely prescribe medications that will thin your blood and make it less likely to clot, such as pills or injections. Certain thrombolytics (“clot busting”) medicines can even break apart an existing clot and dissolve it entirely.
How to Treat Blood Clots in Lungs
Commonly, blood thinners or anticoagulants are used. These medications stop clots from growing and forming as your body dissolves them.
Heparin, often given intravenously or via injection, acts fast. It’s coupled with oral anticoagulants like warfarin until they take effect.
Usually, the goal is for your body to dissolve the clot naturally. If not, more serious measures might be needed. Treatments include:
- Clot Dissolvers: Thrombolytics, used for dire cases, can cause sudden, severe bleeding.
- Embolectomy: Rarely, surgery is considered. For large, life-threatening clots, a catheter might remove it through blood vessels.
Besides medical treatment, lifestyle changes help prevent clots. Regular exercise, hydration, no tobacco, uncrossed legs, and compression stockings enhance leg blood flow. Reduce risks by discussing with your healthcare provider, especially if you or family have clot history.
Symptoms
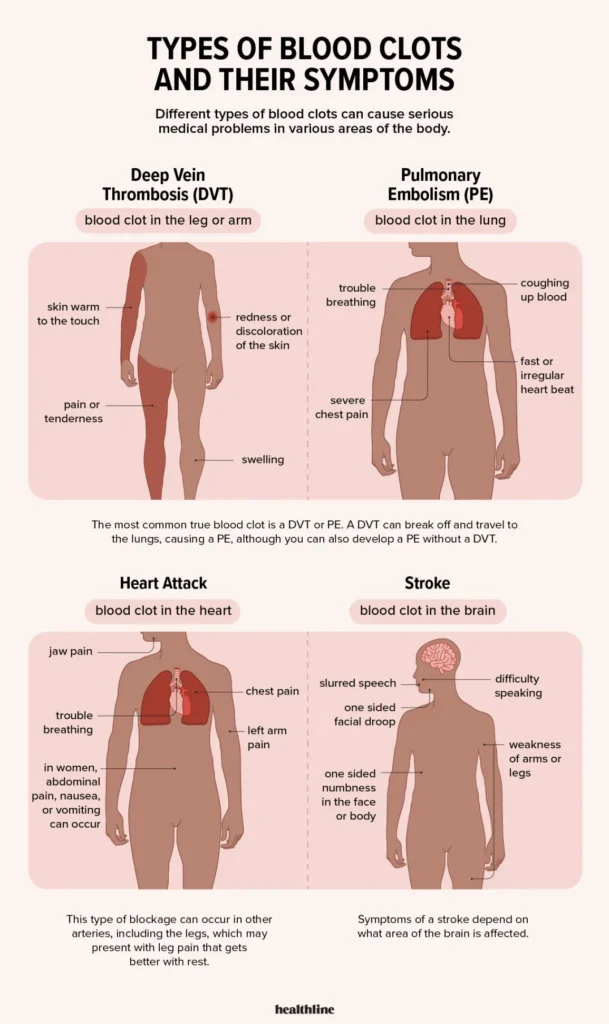
Blood clots in the lungs, commonly referred to as pulmonary embolisms (PE), are rare but serious conditions. PEs block oxygen-rich blood flow, leading to heart failure or chronic shortness of breath. They usually develop in your deep veins in legs but can sometimes break free and travel directly into lungs – an urgent medical situation in which immediate medical advice must be sought immediately.
Your doctor will prescribe anticoagulant therapy medicines to thin your blood and decrease the likelihood of future clot formation, and, if applicable, use other drugs known as thrombolytic therapy to dissolve any large, life-threatening PEs in your lungs.
NYU Langone specialists also use minimally invasive approaches that involve inserting a thin tube, known as a catheter, into a vein in your groin or arm and into an artery in your lungs where the clot resides. From there, doctors use this catheter to retrieve or break up the clot or administer medicine directly targeting it.
Diagnosis
Blood clots in the lungs are generally identified through symptoms and medical history. Your doctor may also conduct lung function tests and the D-dimer blood test, which checks for signs that the body is breaking down the clot.
NYU Langone doctors often treat pulmonary embolisms using anticoagulant medicines and clot-busting agents. These reduce the risk of new clot formation while keeping existing ones from growing bigger.
A catheter-directed thrombolysis (DVT) procedure may be necessary in some instances in order to quickly and efficiently treat PEs that have grown large enough that require removal quickly. Your physician will insert a thin tube into your vein and move it toward the clot before administering medicine directly onto it to break up and dissolve it.
Most individuals diagnosed with DVT or PE must take anticoagulant medicines for at least three months; in some instances, doctors may recommend it longer-term or even permanently depending on your medical history and risk of blood clots.

Treatment
Doctors use anticoagulants or “blood thinners” to prevent new clots from forming and break up existing ones. Their choice will depend on factors like where and size of existing clots as well as your risk for further ones in future.
A blood clot may also lead to serious health conditions like pulmonary hypertension, which raises blood pressure in vessels leading to your lungs and can result in sudden heart failure, low oxygen levels, or even sudden death if left untreated.
Your provider may ask about the history of blood clotting disorders in your family and assess symptoms like chest pain or shortness of breath. A noninvasive test called duplex ultrasonography (DUO) uses sound waves to scan for blood clots in leg or arm veins – this allows doctors to spot DVT before it causes PE.
Prevention
Blood clots tend to form more frequently in veins than in arteries due to slower blood flow in veins and their increased volume containing deoxygenated blood after injury or trauma. Clots may also form due to narrowing of vessel walls (known as stenosis).
Our doctors specialize in DVT/PE prevention by creating an individualized treatment plan which may include medication. They will review your medical history to assess any predisposition towards blood clots as well as conduct blood tests to measure how much oxygen your blood carries.
Clots may be removed with the aid of a thin, flexible tube known as a catheter that is guided through an incision in your groin or neck and into an artery that leads to your lungs.
Through catheter-directed percutaneous thrombolysis, doctors use medication in the catheter to deliver directly into your clot. For larger clots, surgery may be necessary.
What Are the Symptoms of a Blood Clot in the Lungs

Symptoms of a lung blood clot (pulmonary embolism) differ by clot severity and individual. Common signs include:
- Breath Shortness: Suddenly occurs, even at rest, could worsen during activity.
- Chest Pain: Often sharp, resembling heart attack pain, felt with deep breaths, coughs, bends.
- Cough: May bring cough with bloody mucus.
- Heartbeat Changes: Fast or irregular pulse could be noticed.
- Lightheadedness: May feel dizzy or faint.
- Excessive Sweating: Could lead to profuse sweating.
- Leg Pain/Swelling: In certain cases, leg clot (deep vein thrombosis) reaching lungs causes symptoms—leg pain, swelling.
- Wheezing: Some may experience wheezing.
Remember, not everyone with lung clot will show all symptoms, and some may not show any. Suspect clot or experience these signs? Urgently seek medical help.
What Are the Risk Factors for Developing Blood Clots in the Lungs
The risk factors for developing lung blood clots (pulmonary embolism) are:
- Deep Vein Thrombosis (DVT): History of DVT increases pulmonary embolism risk. DVT often occurs in legs.
- Prolonged Immobility: Extended stillness, like during hospitalization, bed rest, flights, or drives, heightens risk.
- Hypercoagulability: Certain factors, like birth control, smoking, cancer, surgery, or pregnancy, make blood clot-prone.
- Family History: Blood clot history in family raises pulmonary embolism risk.
- Age: Risk rises with age; every decade after 60, risk doubles.
- Surgery and Injury: Operations, especially joint replacements, and leg injuries increase risk.
- Limited Mobility: Rest, travel, paralysis heighten clot risk.
- Medical Conditions: Heart failure, COPD, high blood pressure, stroke, and inflammatory bowel disease raise risk.
- Cancer and Treatment: Cancer or cancer therapies increase clot risk.
Having these factors doesn’t guarantee lung clots. Awareness helps prevent and manage embolism. Concerned about risk? Consult your healthcare provider.
How Long Does It Take To Recover From a Blood Clot in the Lungs

Recovering from a lung blood clot (pulmonary embolism) varies based on situations. Generally, it takes weeks to months.
Hospital stay and clot-preventing meds might be needed for over three months. Most fully recover, but some face lingering symptoms, like breath shortage.
Recovery varies, some facing prolonged symptoms. Persistent breathing issues six months post-clot need doctor’s attention for possible CTEPH.
Medication to prevent clots is vital during treatment. Anticoagulants, or “blood thinners,” prevent clot growth as body dissolves it.
After a pulmonary embolism, light activities like walking and housework are possible. Rest, follow meds, and doctor’s advice to monitor recovery and prevent future clots.














